Getting pregnant at 35 risks refers to potential health concerns associated with conceiving a child at or after the age of 35. For instance, women in this age group are more likely to experience pregnancy complications such as gestational diabetes or premature birth.
Understanding these risks is crucial as they can impact both the mother and the baby’s well-being. Advanced maternal age has been a subject of research, leading to advancements in prenatal care and fertility treatments, enabling women to make informed decisions about family planning.
This article delves into the medical, social, and lifestyle factors surrounding getting pregnant at 35 and beyond, providing comprehensive information to help navigate this important life stage.
Getting Pregnant at 35
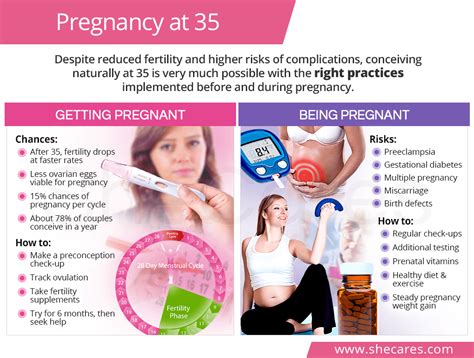
Understanding the risks associated with getting pregnant at 35 and beyond is crucial for informed decision-making. These risks encompass various aspects, including:
- Fertility decline
- Gestational diabetes
- Preeclampsia
- Premature birth
- Low birth weight
- Chromosomal abnormalities
- Multiple pregnancies
- Cesarean delivery
- Postpartum recovery
These aspects highlight the importance of prenatal care, genetic counseling, and lifestyle modifications for women considering pregnancy at 35 or older. By understanding these risks and taking appropriate measures, women can increase their chances of having a healthy pregnancy and delivery.
Fertility decline
Fertility decline is a significant component of the risks associated with getting pregnant at 35 and beyond. As women age, their fertility naturally decreases due to a decline in the quality and quantity of eggs. This decline begins gradually in the late 20s and becomes more pronounced after 35.
The primary cause of fertility decline with age is the depletion of ovarian reserve. Ovarian reserve refers to the number of eggs a woman has. Each month, a woman’s ovaries release an egg during ovulation. As a woman ages, her ovarian reserve diminishes, and the eggs that remain are more likely to have chromosomal abnormalities.
The impact of fertility decline on getting pregnant at 35 can be significant. Women over 35 are less likely to conceive each month compared to younger women. They may also require more cycles of fertility treatments, such as IVF, to achieve pregnancy.
Understanding the connection between fertility decline and getting pregnant at 35 is crucial for women who are considering pregnancy in their late 30s or beyond. By being aware of the risks, women can make informed decisions about their reproductive health and explore options such as fertility preservation or egg freezing if desired.
Gestational diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. It usually appears in the second or third trimester and goes away after the baby is born. However, women who have had gestational diabetes are at an increased risk of developing type 2 diabetes later in life.
Gestational diabetes is a serious condition that can affect both the mother and the baby. For the mother, gestational diabetes can increase the risk of preeclampsia, premature birth, and cesarean delivery. For the baby, gestational diabetes can increase the risk of macrosomia (large birth weight), hypoglycemia (low blood sugar), and respiratory distress syndrome.
The exact cause of gestational diabetes is unknown, but it is thought to be related to changes in hormone levels during pregnancy. These changes can make it difficult for the body to use insulin effectively, which can lead to high blood sugar levels.
Gestational diabetes is a common condition, affecting up to 10% of pregnant women. It is more common in women who are over 35, overweight or obese, or have a family history of diabetes.
If you are pregnant and over 35, it is important to be aware of the risks of gestational diabetes and to talk to your doctor about ways to reduce your risk.
Preeclampsia
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and protein in the urine. It usually develops after 20 weeks of pregnancy and can lead to serious health problems for both the mother and the baby if left untreated.
Preeclampsia is more common in women who are pregnant for the first time, women who are over 35, and women who have certain medical conditions, such as high blood pressure, diabetes, or kidney disease. The exact cause of preeclampsia is unknown, but it is thought to be related to problems with the placenta.
Preeclampsia can have a significant impact on the health of both the mother and the baby. For the mother, preeclampsia can increase the risk of seizures, stroke, and organ damage. For the baby, preeclampsia can lead to premature birth, low birth weight, and other health problems.
There is no cure for preeclampsia, but it can be managed with medication and lifestyle changes. In severe cases, the baby may need to be delivered early.
If you are pregnant and over 35, it is important to be aware of the risks of preeclampsia and to talk to your doctor about ways to reduce your risk.
Premature birth
Premature birth, also known as preterm birth, is a significant risk associated with getting pregnant at 35 and beyond. It refers to the delivery of a baby before 37 weeks of gestation. Premature birth can have serious health implications for both the mother and the baby, including an increased risk of infant mortality, respiratory problems, and developmental delays.
The connection between premature birth and getting pregnant at 35 risks is multifaceted. As women age, the quality of their eggs declines, and the risk of chromosomal abnormalities increases. These factors can contribute to placental problems, which can lead to premature birth. Additionally, older women are more likely to have underlying health conditions, such as high blood pressure or diabetes, which can also increase the risk of premature birth.
Premature birth is a critical component of getting pregnant at 35 risks due to its potential impact on the health and well-being of both the mother and the baby. It is estimated that approximately 12% of babies born to women over 35 are premature, compared to 8% of babies born to women under 35.
Understanding the connection between premature birth and getting pregnant at 35 risks is crucial for women who are considering pregnancy in their late 30s or beyond. By being aware of the risks, women can make informed decisions about their reproductive health and take steps to reduce their risk of premature birth, such as maintaining a healthy weight, managing underlying health conditions, and receiving regular prenatal care.
Low birth weight
Low birth weight is a significant aspect of getting pregnant at 35 risks, as it can have short- and long-term health implications for the baby. It refers to infants born weighing less than 2,500 grams (5 pounds 8 ounces). This condition is more prevalent in pregnancies involving older mothers due to various factors related to the aging process and associated health risks.
- Placental Insufficiency
As women age, the placenta, which provides oxygen and nutrients to the fetus, may not function optimally. This can lead to restricted fetal growth and low birth weight.
- Preeclampsia
Preeclampsia, a pregnancy complication characterized by high blood pressure and protein in the urine, is more common in older pregnancies. It can restrict blood flow to the placenta, affecting fetal growth and potentially resulting in low birth weight.
- Intrauterine Growth Restriction
Intrauterine growth restriction (IUGR) occurs when the fetus does not grow as expected within the uterus. It can be caused by various factors, including placental insufficiency and preeclampsia, both of which are more prevalent in older pregnancies.
- Maternal Health Conditions
Older mothers are more likely to have underlying health conditions, such as high blood pressure or diabetes, which can affect placental function and fetal growth, increasing the risk of low birth weight.
Low birth weight can have significant implications for the baby’s health. These infants are more susceptible to respiratory problems, infections, and developmental delays. They may also be at an increased risk of chronic health conditions, such as cardiovascular disease and diabetes, later in life. Therefore, understanding the connection between low birth weight and getting pregnant at 35 risks is crucial for expectant mothers and healthcare providers to ensure proper prenatal care and monitoring to mitigate these risks and promote optimal fetal growth.
Chromosomal abnormalities
Chromosomal abnormalities are a significant aspect of getting pregnant at 35 risks, as they can lead to various health issues for the baby. These abnormalities occur when there is an error in the number or structure of chromosomes, which are the structures in cells that carry genetic information.
- Down syndrome
Down syndrome is a genetic disorder caused by the presence of an extra copy of chromosome 21. It can lead to intellectual disability, developmental delays, and physical features such as a flattened facial profile, small stature, and an enlarged tongue. - Trisomy 18
Trisomy 18 is a genetic disorder caused by the presence of an extra copy of chromosome 18. It is a serious condition that can lead to multiple birth defects and intellectual disability. Most babies with trisomy 18 die before birth or shortly after. - Turner syndrome
Turner syndrome is a genetic disorder that affects only females. It is caused by the absence of one of the two X chromosomes. Turner syndrome can lead to short stature, infertility, and other health problems. - Klinefelter syndrome
Klinefelter syndrome is a genetic disorder that affects only males. It is caused by the presence of an extra X chromosome. Klinefelter syndrome can lead to tall stature, infertility, and learning disabilities.
Chromosomal abnormalities can have a significant impact on the health and well-being of a child. Therefore, it is important for women over 35 to be aware of the risks and to talk to their doctor about genetic screening and counseling.
Multiple pregnancies
Multiple pregnancies, also known as multifetal pregnancies, involve carrying more than one fetus at a time. This condition is more common in women who get pregnant at 35 and beyond due to several factors associated with the aging reproductive system and fertility treatments.
One of the main causes of multiple pregnancies in older women is the use of fertility treatments, such as in vitro fertilization (IVF). IVF involves stimulating the ovaries to produce multiple eggs, which are then fertilized in a laboratory and implanted into the uterus. This process increases the chances of conceiving twins, triplets, or even more babies.
Multiple pregnancies carry a higher risk of complications for both the mother and the babies. These risks include premature birth, low birth weight, gestational diabetes, preeclampsia, and cesarean delivery. Additionally, multiple pregnancies can strain the mother’s body, leading to fatigue, back pain, and other physical discomfort.
For women over 35 who are considering pregnancy, it is important to understand the risks associated with multiple pregnancies. They should discuss these risks with their doctor and make informed decisions about their reproductive health and fertility treatments.
Cesarean delivery
Cesarean delivery, also known as C-section, is a surgical procedure to deliver a baby through an incision in the abdomen and uterus. It is a common procedure, especially among women who are getting pregnant at 35 and beyond. There are several factors that contribute to the increased risk of Cesarean delivery in older, including:
- Advanced maternal age
As women age, their uterine muscles become less elastic, which can make it more difficult to deliver a baby vaginally. - Multiple pregnancies
Women who are pregnant with twins, triplets, or more are more likely to require a cesarean delivery. - Placenta previa
This condition occurs when the placenta implants in the lower part of the uterus, blocking the cervix. It can lead to bleeding and other complications during labor, making a cesarean delivery necessary. - Fetal distress
If the baby is in distress during labor, a cesarean delivery may be necessary to protect the baby’s health.
Cesarean delivery is a major surgery, and it carries some risks for both the mother and the baby. These risks include bleeding, infection, and blood clots. However, cesarean delivery is a safe and effective procedure when it is necessary to protect the health of the mother and the baby.
Postpartum recovery
Postpartum recovery is a critical component of getting pregnant at 35 risks. As women age, their bodies take longer to recover from childbirth. This is due to several factors, including hormonal changes, decreased muscle tone, and weakened pelvic floor muscles.
Prolonged postpartum recovery can lead to a number of complications, including postpartum depression, incontinence, and pelvic organ prolapse. These complications can have a significant impact on a woman’s quality of life and can make it difficult to care for a newborn.
There are a number of things that women can do to improve their postpartum recovery. These include:
- Getting plenty of rest
- Eating a healthy diet
- Exercising regularly
- Seeing a physical therapist or chiropractor
- Taking care of their mental health
Getting Pregnant at 35
This FAQ section addresses common queries and clarifies aspects related to the risks of getting pregnant at 35 and beyond.
Question 1: What are the main risks associated with getting pregnant at 35?
Answer: As women age, they are more likely to experience fertility decline, gestational diabetes, preeclampsia, premature birth, low birth weight, chromosomal abnormalities, multiple pregnancies, cesarean delivery, and prolonged postpartum recovery.
Question 2: How does fertility decline affect getting pregnant at 35?
Answer: Fertility gradually decreases with age, especially after 35, due to a decline in the quality and quantity of eggs. This can make it more challenging to conceive and may require fertility treatments.
Question 3: What is gestational diabetes and why is it a risk for older pregnancies?
Answer: Gestational diabetes is a type of diabetes that develops during pregnancy and is more common in women over 35. It is linked to changes in hormone levels that affect the body’s ability to use insulin.
Question 4: How can I reduce the risk of premature birth if I’m pregnant at 35 or older?
Answer: Maintaining a healthy weight, managing underlying health conditions, receiving regular prenatal care, and following your doctor’s recommendations can help reduce the risk of premature birth.
Question 5: What are the potential health implications of low birth weight for babies born to older mothers?
Answer: Babies born with low birth weight may have an increased risk of respiratory problems, infections, developmental delays, and chronic health conditions later in life.
Question 6: How can I improve my postpartum recovery after getting pregnant at 35 or older?
Answer: Getting plenty of rest, eating a healthy diet, exercising regularly, and seeking professional help from a physical therapist or chiropractor can aid in postpartum recovery.
Summary: Understanding the risks associated with getting pregnant at 35 and beyond is essential for informed decision-making. By being aware of potential complications and taking appropriate measures, women can increase their chances of a healthy pregnancy and delivery.
Transition: As we delve further into the topic, the next section will explore strategies for managing these risks and optimizing reproductive health for women over 35.
Tips for Managing Risks of Getting Pregnant at 35 and Beyond
This section provides practical, evidence-based tips to help women over 35 navigate the risks associated with pregnancy and improve their reproductive health.
Tip 1: Prioritize Preconception Care
Start prenatal care before conceiving to manage underlying health conditions, optimize nutrition, and reduce the risk of complications.
Tip 2: Maintain a Healthy Weight
Obesity increases the risk of gestational diabetes, preeclampsia, and cesarean delivery. Aim for a healthy BMI before and during pregnancy.
Tip 3: Manage Chronic Conditions
Women with pre-existing conditions like diabetes or hypertension should work closely with their healthcare providers to manage these conditions and minimize risks.
Tip 4: Consider Fertility Preservation
If you plan to delay pregnancy beyond your early 30s, consider fertility preservation options like egg freezing to preserve your fertility potential.
Tip 5: Seek Genetic Counseling
Genetic counseling can assess your risk of having a baby with chromosomal abnormalities and provide guidance on reproductive options.
Tip 6: Follow a Nutritious Diet
Ensure adequate intake of folic acid, iron, and calcium. A balanced diet supports fetal growth and reduces the risk of pregnancy complications.
Tip 7: Exercise Regularly
Regular physical activity promotes overall health, improves circulation, and reduces the risk of gestational diabetes and other pregnancy-related complications.
Tip 8: Quit Smoking and Limit Alcohol
Smoking and excessive alcohol consumption can harm both the mother and the baby. Quit smoking and minimize alcohol intake during pregnancy.
By implementing these tips and working closely with healthcare providers, women over 35 can proactively manage the risks associated with pregnancy and increase their chances of a healthy pregnancy and delivery.
The following section will delve into the impact of lifestyle choices on pregnancy outcomes, highlighting the importance of informed decision-making and self-care during this critical life stage.
Conclusion
This article has explored the multifaceted risks associated with getting pregnant at 35 and beyond. As women age, they face an increased likelihood of fertility decline, gestational diabetes, preeclampsia, premature birth, and other complications. Understanding these risks is crucial for informed decision-making and proactive management.
Key points to consider include: prioritizing preconception care, maintaining a healthy weight, managing chronic conditions, and considering fertility preservation options. Additionally, adopting a nutritious diet, engaging in regular exercise, quitting smoking, and limiting alcohol consumption can significantly improve pregnancy outcomes.
Getting pregnant at 35 and beyond requires careful planning, optimization of reproductive health, and a collaborative approach with healthcare providers. By embracing informed decision-making and self-care, women can increase their chances of a healthy pregnancy and delivery, ensuring the well-being of both themselves and their future children.