Getting pregnant at age 35 is a common concern for women. The question “how long will it take me to get pregnant at 35” weighs heavily on many people’s minds due to age-related fertility decline.
Understanding this concept is vital for family planning and reproductive health decisions. Pregnancy rates decrease with age, particularly after 35, highlighting its relevance. It also provides valuable insights into the biological processes involved in conception. Historically, this notion has fueled research and advancements in assisted reproductive technologies.
This article delves into various factors influencing pregnancy chances at 35, including age-related physiological changes, lifestyle choices, and medical interventions. It aims to provide comprehensive information and guidance to help individuals make informed decisions about their reproductive goals.
How Long Will It Take Me to Get Pregnant at 35?
Understanding the key aspects that influence pregnancy chances at age 35 is crucial for reproductive planning. These aspects encompass various dimensions, including biological factors, lifestyle choices, and medical interventions.
- Age-related fertility decline
- Ovarian reserve
- Lifestyle choices
- Medical history
- Sperm health
- Assisted reproductive technologies
- Emotional well-being
- Support systems
- Financial considerations
These aspects are interconnected and can significantly impact the time it takes to conceive. Age-related fertility decline, for instance, affects the quality and quantity of eggs, reducing pregnancy chances. Lifestyle choices such as smoking, excessive alcohol consumption, and inadequate nutrition can further diminish fertility. Medical interventions like IVF and IUI can increase pregnancy rates, while emotional support and financial stability contribute to a positive pregnancy journey.
Age-related fertility decline
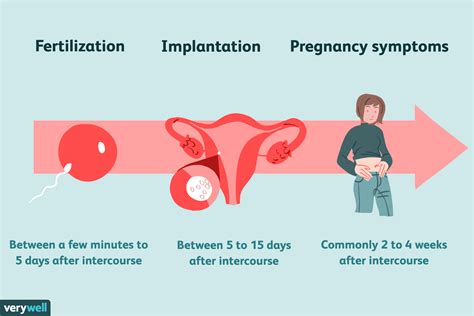
Age-related fertility decline is a significant factor that influences the time it takes to get pregnant at 35. As women age, their fertility naturally declines due to several physiological changes.
- Diminished ovarian reserve
The ovarian reserve refers to the number of eggs a woman has. With age, the ovarian reserve decreases, leading to a decline in the quality and quantity of eggs.
- Reduced egg quality
The quality of eggs declines with age, affecting their ability to be fertilized and implant successfully.
- Hormonal changes
Age-related hormonal changes, such as decreased estrogen and progesterone levels, can impact ovulation and the menstrual cycle, making it more challenging to conceive.
- Increased risk of miscarriage
Women over 35 have a higher risk of miscarriage due to chromosomal abnormalities in eggs.
These factors collectively contribute to the age-related decline in fertility, which is a key consideration when determining how long it may take to get pregnant at 35.
Ovarian reserve
Ovarian reserve plays a crucial role in determining how long it takes to get pregnant at 35. It refers to the number and quality of eggs a woman has. As women age, their ovarian reserve naturally declines, which affects their fertility.
The decline in ovarian reserve is primarily caused by the aging process. As women reach their mid-30s, the number of eggs in their ovaries begins to decrease. This reduction in egg count is accompanied by a decline in egg quality. The eggs that remain may be more likely to have chromosomal abnormalities, which can increase the risk of miscarriage.
The impact of ovarian reserve on fertility is significant. Women with a lower ovarian reserve have a lower chance of getting pregnant each month. They may also be more likely to experience infertility and require fertility treatments to conceive.
Understanding ovarian reserve can help women make informed decisions about their reproductive health. Women who are concerned about their fertility may want to consider having their ovarian reserve tested. This test can provide valuable information about their chances of getting pregnant naturally and may help them plan for the future.
In summary, ovarian reserve is a critical component of female fertility. The decline in ovarian reserve with age is a major factor that influences how long it takes to get pregnant at 35. Understanding ovarian reserve can help women make informed decisions about their reproductive health and plan for the future.
Lifestyle choices
Lifestyle choices significantly impact how long it takes to get pregnant at 35. Maintaining a healthy weight, engaging in regular exercise, and adopting a balanced diet can improve fertility and increase the chances of conception.
Obesity can disrupt ovulation and hormone production, making it more challenging to get pregnant. Exercise helps regulate weight, reduce stress, and improve overall health, all of which contribute to better fertility outcomes. A healthy diet rich in fruits, vegetables, and whole grains provides essential nutrients for both the woman and the developing fetus.
Conversely, smoking, excessive alcohol consumption, and drug use can harm fertility. Smoking damages eggs and reduces ovarian reserve, while alcohol can interfere with ovulation and implantation. Drug use can disrupt hormone production and overall health, negatively affecting fertility.
Making healthy lifestyle choices can significantly improve fertility and increase the chances of getting pregnant at 35. By maintaining a healthy weight, engaging in regular exercise, and adopting a balanced diet, women can optimize their reproductive health and enhance their chances of conception.
Medical history
Medical history plays a significant role in determining how long it takes to get pregnant at 35. It provides valuable insights into potential health conditions or previous medical interventions that may impact fertility.
- Prior pregnancies and birth outcomes
Previous pregnancies, miscarriages, or birth complications can influence current fertility status. A history of premature birth, low birth weight, or cesarean section may warrant further evaluation.
- Sexually transmitted infections (STIs)
Untreated STIs can lead to pelvic inflammatory disease (PID) or other reproductive tract infections, potentially causing infertility or pregnancy complications.
- Chronic health conditions
Underlying health conditions, such as diabetes, thyroid disorders, or autoimmune diseases, can affect fertility and pregnancy outcomes. Proper management of these conditions is crucial.
- Gynecological surgeries
Previous surgeries, such as myomectomy (fibroid removal) or hysteroscopic procedures, may impact uterine and ovarian function, affecting fertility.
Understanding medical history allows healthcare providers to assess potential risk factors, provide appropriate counseling, and recommend necessary interventions to improve fertility and pregnancy chances.
Sperm health
Sperm health plays a crucial role in determining how long it takes to get pregnant at 35. Male fertility is influenced by various factors, including sperm count, motility, and morphology. These factors can significantly impact the likelihood of conception.
Sperm count refers to the number of sperm present in a single ejaculate. A low sperm count, also known as oligospermia, can reduce the chances of fertilization. Sperm motility is the ability of sperm to move effectively, which is essential for reaching and penetrating the egg. Impaired sperm motility, known as asthenozoospermia, can hinder fertilization.
Sperm morphology refers to the shape and structure of sperm. Abnormal sperm morphology, known as teratozoospermia, can affect sperm’s ability to fertilize the egg. These factors collectively contribute to male infertility and can prolong the time it takes to conceive.
Understanding sperm health is crucial for couples trying to conceive at 35. Men with concerns about their fertility may consider seeking medical evaluation to assess their sperm health and address any underlying issues that may be affecting their ability to conceive.
Assisted reproductive technologies
Assisted reproductive technologies (ARTs) play a significant role in addressing infertility and improving the chances of pregnancy, particularly for women over 35. These technologies offer various options to help individuals conceive, including in vitro fertilization (IVF), intrauterine insemination (IUI), and surrogacy.
For women facing age-related fertility decline, ARTs provide a means to overcome challenges associated with diminished ovarian reserve and egg quality. IVF, for instance, involves retrieving eggs from the ovaries, fertilizing them with sperm in a laboratory setting, and transferring the resulting embryos back into the uterus. This process bypasses natural conception and increases the likelihood of pregnancy.
ARTs have revolutionized the landscape of reproductive medicine by expanding the possibilities for individuals to have children despite age or other fertility challenges. They offer hope and support to those who are struggling to conceive and play a crucial role in helping people achieve their family-building goals.
Emotional well-being
Emotional well-being plays a crucial role in the journey to conceive at 35. It encompasses various facets that can significantly impact a woman’s physical and mental health, ultimately affecting her fertility and pregnancy outcomes.
- Stress management
Chronic stress can disrupt hormonal balance and ovulation, hindering conception. Managing stress through techniques like yoga, meditation, or spending time in nature can promote relaxation and improve fertility.
- Positive self-image
A positive body image and high self-esteem can contribute to better fertility outcomes. Embracing your body and practicing self-care can reduce stress and promote overall well-being, which is beneficial for conception.
- Emotional support
Having a strong support system of family, friends, or a therapist can provide emotional stability and reduce anxiety during the fertility journey. Sharing experiences and seeking encouragement can foster a sense of belonging and reduce stress levels.
- Mind-body connection
The mind and body are deeply interconnected. Practicing mindfulness, relaxation techniques, or acupuncture can promote a sense of calm and balance, which can have a positive impact on fertility.
By addressing emotional well-being and incorporating these facets into your lifestyle, you can create a more favorable environment for conception and improve your overall health during the journey to pregnancy at 35.
Support systems
Support systems play a crucial role in the journey to conceive at 35. They provide emotional stability, reduce stress, and offer valuable resources and guidance throughout the process.
Having a strong support system can positively impact fertility outcomes. Emotional support from family, friends, or a therapist can help manage stress levels, which can disrupt hormonal balance and ovulation. Sharing experiences and seeking encouragement within a support network can foster a sense of belonging and reduce anxiety, creating a more favorable environment for conception.
Moreover, support systems can provide practical assistance during the fertility journey. They can accompany you to medical appointments, offer childcare for other children, or simply lend a listening ear. This practical support can alleviate the burden of infertility and allow you to focus on your physical and emotional well-being.
In summary, support systems are a critical component of the journey to conceive at 35. They provide emotional stability, reduce stress, and offer valuable resources and guidance. By leveraging the power of support systems, individuals can navigate the challenges of infertility with greater resilience and improve their chances of achieving pregnancy.
Financial considerations
Financial considerations play a significant role in the journey to conceive at 35. The costs associated with fertility treatments, prenatal care, delivery, and childcare can be substantial, and these expenses can impact the timeline of getting pregnant.
For couples who require assisted reproductive technologies (ARTs), such as IVF or IUI, the financial burden can be particularly high. These treatments often involve multiple rounds of procedures, each with its own associated costs. Additionally, the success rates of ARTs can vary, meaning that couples may need to undergo multiple rounds before achieving pregnancy, further increasing the financial strain.
Beyond the direct costs of fertility treatments, there are also indirect financial considerations to take into account. For example, women who undergo ARTs may need to take time off work for appointments and procedures, which can result in lost income. Additionally, the emotional stress of infertility can lead to reduced work productivity or job loss, further exacerbating financial challenges.
It is important for couples to carefully consider their financial situation before embarking on the journey to conceive at 35. Open and honest communication about financial expectations and limitations can help couples make informed decisions about their treatment options and timeline.
Frequently Asked Questions about Getting Pregnant at 35
This section addresses frequently asked questions about getting pregnant at 35, providing concise and informative answers to common concerns and misconceptions.
Question 1: How does age affect fertility at 35?
After 35, women experience a gradual decline in fertility due to a decrease in egg quantity and quality, making it more challenging to conceive.
Question 2: What are the chances of getting pregnant naturally at 35?
The chances of getting pregnant naturally at 35 are about 12% per menstrual cycle, which is lower than in younger women.
Question 3: How long does it usually take to get pregnant at 35?
It can take longer to get pregnant at 35 compared to younger ages. About 80% of couples who are actively trying will conceive within a year, while others may take longer or require fertility treatments.
Question 4: What are the lifestyle factors that can affect fertility at 35?
Maintaining a healthy weight, engaging in regular exercise, and adopting a balanced diet can improve fertility and increase the chances of conception.
Question 5: What medical conditions can impact fertility at 35?
Underlying health conditions, such as thyroid disorders, endometriosis, or pelvic inflammatory disease, can affect fertility and should be addressed.
Question 6: What are the options for assisted reproductive technologies (ARTs) at 35?
ARTs, such as IVF or IUI, can increase the chances of pregnancy for women with age-related fertility decline.
In summary, getting pregnant at 35 requires a comprehensive understanding of age-related fertility changes, lifestyle factors, and medical conditions. While the journey may take longer than at younger ages, there are various options available to support conception.
Further discussion in the following sections will delve into the specific factors that influence fertility at 35 and explore strategies to optimize reproductive health.
Tips for Getting Pregnant at 35
Navigating fertility at 35 requires a proactive approach. Here are some practical tips to help you optimize your chances of conception:
Tip 1: Track Your Cycle
Monitoring your menstrual cycle can help you identify your fertile window and plan intercourse accordingly.
Tip 2: Maintain a Healthy Weight
Being overweight or underweight can impact hormone balance and ovulation.
Tip 3: Exercise Regularly
Moderate exercise promotes overall health and may improve fertility.
Tip 4: Adopt a Balanced Diet
Consuming a diet rich in fruits, vegetables, and whole grains provides essential nutrients for reproductive health.
Tip 5: Manage Stress
Chronic stress can disrupt hormone production and affect fertility.
Tip 6: Quit Smoking
Smoking damages eggs and reduces ovarian reserve.
Tip 7: Limit Alcohol Consumption
Excessive alcohol intake can interfere with ovulation and implantation.
Tip 8: Consider Fertility Supplements
Prenatal vitamins and supplements like folic acid and CoQ10 may support reproductive health.
Summary of key takeaways or benefits
By implementing these tips, you can enhance your overall well-being, optimize your fertility, and increase your chances of conceiving at 35.
Transition to the article’s conclusion
These tips serve as a foundation for your fertility journey. Remember that every woman’s experience is unique, and it is always advisable to consult with a healthcare professional to discuss your specific needs and develop a personalized plan.
Conclusion
Understanding the intricacies of getting pregnant at 35 is a multifaceted exploration that encompasses biological factors, lifestyle choices, and emotional well-being. This article has delved into the complexities of this topic, providing valuable insights into the factors that influence conception chances and the strategies that can optimize fertility.
Key takeaways from this exploration include the gradual decline in fertility with age, the importance of lifestyle modifications, and the role of emotional well-being in the fertility journey. These interconnected aspects highlight the need for a comprehensive approach to maximizing pregnancy chances at 35.